The journey of understanding the effects of selective serotonin reuptake inhibitors (SSRIs) has been fraught with both hope and controversy. Widely prescribed for the treatment of anxiety and depression, SSRIs like escitalopram are utilized by millions worldwide. However, their mechanisms and long-term efficacy remain largely enigmatic. Recent research led by psychologist Vibeke Dam from Copenhagen University sheds light on these issues, emphasizing the cognitive alterations that may accompany SSRI treatment. This article delves into the findings of the study, critiques the methodology and implications, and reflects on the broader implications for psychiatry.
Study Design and Methodology
The study conducted by Dam and her colleagues analyzed a group of 90 patients diagnosed with moderate to severe depression. Their approach involved both cognitive assessments and advanced brain imaging techniques to establish a baseline prior to SSRI treatment. Patients were administered escitalopram daily for eight weeks, followed by subsequent cognitive evaluations and brain scans. This methodology seemingly offers a robust examination of the interplay between medication and cognitive functioning. However, the reliance on a single SSRI and a non-placebo control raises fundamental questions about the robustness of the findings.
While intriguing, the chosen design does not unequivocally demonstrate that observed cognitive improvements were due to the medication rather than external variables or natural fluctuations in mood disorder progression. The absence of a control group receiving a placebo limits the ability to attribute these cognitive enhancements directly to SSRI administration, underscoring the necessity for future research employing more stringent controls.
Key Findings and Discoveries
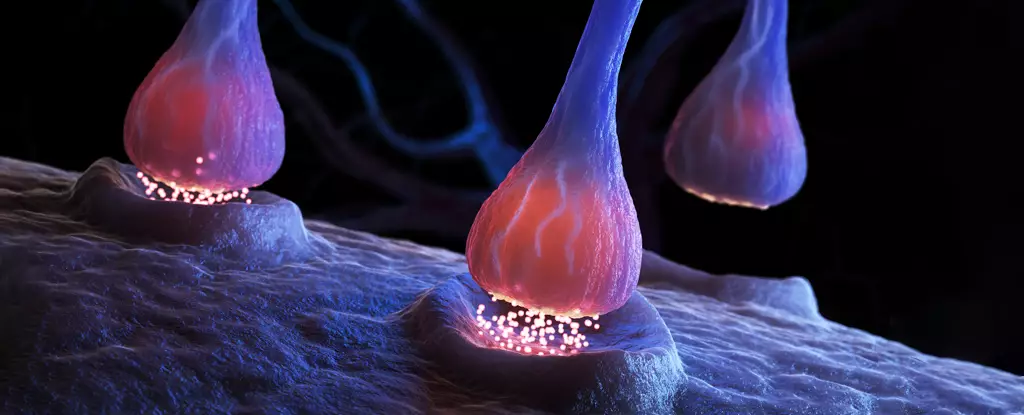
The research yielded some notable results, particularly regarding the effects on cognitive function. Patients exhibited a nearly 10% reduction in serotonin receptors known to be influenced by SSRIs. Surprisingly, those with minimal changes in the 5HT4 receptor displayed the most significant improvement in word recall, suggesting an intricate interplay between receptor activity and cognitive enhancement.
These findings prompt a reevaluation of the established paradigms of how antidepressants function—specifically, the dichotomy between mood improvement and cognitive enhancement raised some eyebrows. While improvements in memory were evident, they did not correspond neatly with mood changes, showcasing a disconnection that remains a puzzle in psychiatric research. This divergence points to the need for a more nuanced understanding of serotonin’s role, as recent arguments challenge the predominant theory that serotonin levels are solely responsible for mood disorders.
Recent investigations have prompted critical scrutiny of SSRIs, with some studies suggesting they do not perform any better than placebo. Furthermore, the concept of serotonin being intricately linked to depression has been increasingly contested. This growing body of literature raises a profound existential crisis regarding the treatment of mood disorders. It invites anxious patients and the medical community alike to reevaluate the foundations of contemporary psychiatric treatment—especially since millions rely on SSRIs to manage their symptoms.
Given these revelations, it is crucial for practitioners to navigate patient treatment plans with caution. If SSRIs can offer cognitive benefits without significantly alleviating mood, we must consider the implications for the therapeutic landscape of depression. It could be argued that SSRIs serve merely as a band-aid rather than a cure, prompting the necessity for a diversified treatment approach embracing both pharmacological and non-pharmacological strategies.
Dam and her colleagues emphasize the need for further exploration of the specific receptor interactions that mediate these cognitive benefits. Their statement highlights a pathway toward personalized psychiatric care, advocating for an approach that tailors treatment options according to individual receptor profiles. However, the ethical concerns around placebos and the intricacies of clinical trials necessitate careful scrutiny.
The need for a comprehensive understanding of antidepressant mechanisms extends beyond SSRIs. Research must delve into alternative treatment modalities—ranging from psychotherapy to lifestyle interventions—that could confer cognitive and emotional benefits without the uncertainties associated with SSRIs.
While the study conducted by Vibeke Dam and her associates provides fascinating insights into the cognitive benefits of SSRIs, it raises more questions than it answers. The complex nature of serotonin receptors and their relationship to cognitive function underscores the pressing need for more extensive research. As we inch closer to unraveling the convoluted mechanisms of antidepressants, it is paramount that we approach the treatment of mood disorders with both caution and innovation. Ultimately, a robust understanding of these dynamics may illuminate the path toward more effective and nuanced treatment strategies for those affected by depression.

Leave a Reply