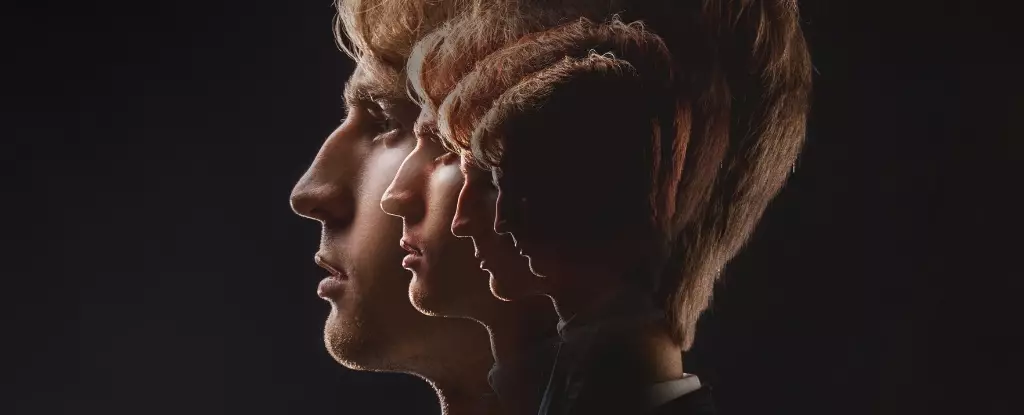
Schizophrenia is not merely a diagnosis; it’s a profound journey into the labyrinth of the human psyche. Affecting over 20 million individuals globally, this severe mental illness dramatically impacts the quality of life for those who succumb to its disorienting grasp. Characterized by pervasive hallucinations and delusions, schizophrenia often takes root during the pivotal years of adolescence and early adulthood, when brain development is at its most crucial. But what causes this debilitating disorder? The search for answers delves into complex interactions of neurobiology, lifestyle, and social factors.
Treatment and understanding schizophrenia have made significant strides, yet the disorder remains shrouded in mental health stigma and misunderstanding. While conventional wisdom links its onset to genetic predispositions and environmental stresses, new research suggests that we may be overlooking a critical aspect: the accelerated ageing of the brain as a contributing factor.
Decoding Brain Development and Ageing
Current theories propose that schizophrenia arises from atypical neurodevelopment during formative years, akin to other neurodevelopmental disorders like autism or ADHD. However, recent advancements point toward a concerning aspect of brain ageing as a potential catalyst in the emergence of this mental health crisis. As revealed in groundbreaking research, the neurofilament light protein (NfL) serves as a crucial biomarker, providing insight into the well-being of individuals with schizophrenia.
NfL is not just a benign protein; it reflects the health status of neurons, the communication cells of the brain. When these neurons undergo damage or degeneration, neurofilament light proteins spill into the bloodstream, revealing the extent of neuronal injury. This phenomenon becomes vital in understanding how schizophrenia correlates with a seemingly accelerated aging process.
Insight from Biomarkers
In the twilight of scientific understanding, biomarkers like NfL provide a tangible measure of neuronal health. Elevated levels of NfL suggest serious neurological implications—often paralleling the symptoms observed in neurodegenerative diseases. Individuals with conditions ranging from Alzheimer’s to Parkinson’s show increased NfL, yet shocking evidence indicates that those with schizophrenia experience an even more pronounced rise in these proteins over time.
What’s particularly alarming is that the study suggests an acceleration in brain ageing not seen in other psychiatric disorders, such as bipolar disorder. This discovery sheds new light on the importance of early diagnosis and intervention both in mental and physical health domains, as the damage inflicted on the brain by schizophrenia may not just be psychological but deeply rooted in biological deterioration.
The Socioeconomic Dimension
Beneath the biological narrative lies a grim socioeconomic context. Individuals diagnosed with schizophrenia frequently have life expectancies that are shockingly 20-30 years lower than the general population. Factors such as social isolation, unemployment, and lifestyle choices compound the difficulties faced by these individuals, culminating in a health crisis that often includes comorbidities like obesity, cardiovascular issues, and chronic pain.
The prevailing stigma tied to mental illness exacerbates these issues and ultimately hinders treatment adherence and lifestyle changes. Many individuals resort to self-medication through illicit drug use to escape the numbing grasp of their symptoms—a vicious cycle that further deteriorates their health and well-being. The implications of such harmful coping mechanisms are significant and deeply troubling, effectively shackling these individuals to a fate worse than mere mental illness.
Redefining Treatment Approaches
In light of this stark reality, it becomes imperative to rethink our strategies for treating schizophrenia. Understanding how brain ageing plays a role could pave the way for groundbreaking therapies that not only focus on symptom mitigation but on the overall health and longevity of the afflicted. The potential to use simple blood tests that measure NfL might completely revolutionize how we approach diagnosis and care for individuals with schizophrenia, allowing for personalized treatment plans that incorporate both mental and physical health strategies.
Establishing a more holistic approach to mental healthcare is crucial in addressing the broader spectrum of health challenges facing individuals living with schizophrenia. Encouraging healthier lifestyles, facilitating social connections, and providing comprehensive treatment for comorbid conditions can have profound effects on improving life expectancy and quality of life for those affected by this complex disorder.
Ultimately, the synergistic relationship between accelerated brain ageing and schizophrenia calls for increased awareness and action from the medical community and society at large. As we stand on the brink of new understandings, it is clear that a multifaceted approach is essential in combating this profound mental illness and reimagining the lives of those entangled in its grasp.

Leave a Reply