The menstrual cycle, often perceived merely through the lens of reproductive health, plays a far more complex role in shaping our overall physiology. A groundbreaking study from the University of California Santa Barbara, led by neuroscientists Elizabeth Rizor and Viktoriya Babenko, provides compelling evidence that hormonal changes during the menstrual cycle can lead to structural and functional shifts in the brain. This underscores a foundational truth: the interplay between our biology and mental processes is intricate and deeply intertwined.
With an astonishing count of approximately 450 menstrual cycles in a typical lifetime, the necessity for comprehensive research into their broader physiological impacts can hardly be overstated. However, the reality is that the discourse surrounding menstruation has long been marred by a lack of in-depth scientific inquiry. The team’s research breaks new ground by emphasizing that the brain itself must be studied as a dynamic entity responding to hormonal flux, not merely as a static structure influenced by cognitive tasks undertaken during these times.
Hormones and Brain Architecture
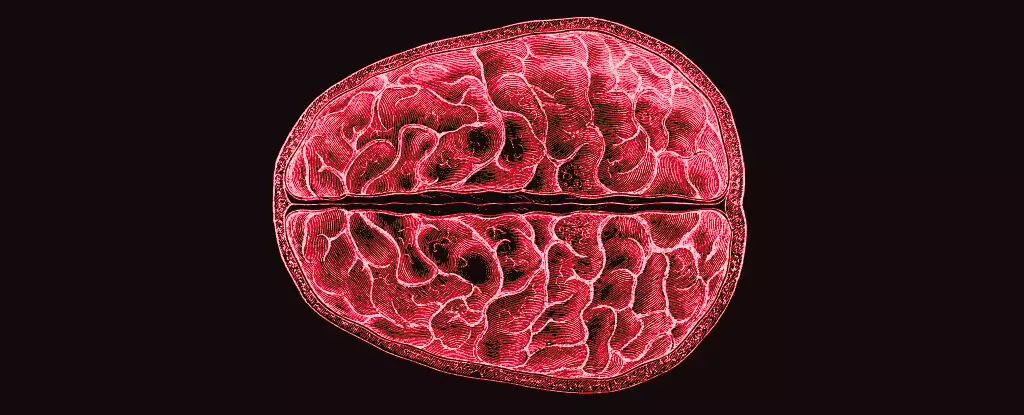
The pioneering study investigates the brain’s structural adaptations in light of hormonal fluctuations taking place during different phases of the menstrual cycle. The researchers employed MRI technology to capture brain changes in thirty participants across three distinct menstrual phases: menses, ovulation, and the mid-luteal phase. The results revealed a fascinating interplay between hormones and brain structure, linking several hormones directly to variations in both gray and white matter.
Notably, the research highlights how the rise of 17β-estradiol just prior to ovulation is correlated with increased white matter changes, suggesting that this hormonal influx enhances the speed at which information is relayed across the brain. White matter, which consists of myelinated neuronal fibers, is essential for optimal information exchange between different brain regions. Furthermore, the study notes that fluctuations in Follicle-Stimulating Hormone (FSH) were behind alterations in gray matter thickness, while the post-ovulation spike in progesterone had contrasting effects, leading to increased tissue volume and a reduction in cerebrospinal fluid.
Beyond Traditional Perspectives
The new insights from this research challenge conventional notions that limit our understanding of hormonal influences on brain function solely to gender-specific brain regions associated with the hypothalamic-pituitary-gonadal (HPG) axis. The findings prompt us to consider that dramatic hormone-driven brain changes may manifest throughout a much broader array of regions than previously recognized. It elucidates the necessity to adopt a more expansive perspective on the entire nervous system, elevating the discussion beyond simplistic, organ-centric models.
Additionally, the connection between these hormonal shifts and the potential for altered neurological functioning raises questions about the psychological ramifications of menstruation. While monthly hormonal fluctuations are a natural occurrence, understanding their neurobiological implications could be pivotal in addressing the mental health issues that disproportionately affect individuals during certain phases of the menstrual cycle. Notably, this could pave the way for more personalized approaches to treating premenstrual syndrome (PMS) and related disorders that often undermine emotional well-being.
A Call for Continued Exploration
As scholars, clinicians, and advocates increasingly recognize the importance of menstrual health, the implications of Rizor and Babenko’s research beckon us to delve deeper. The study shatters the silence surrounding the menstrual cycle’s cerebral effects, propelling it into the realm of crucial scientific inquiry. Future research needs to bridge these newfound understanding gaps, investigating not just the structural changes but also the functional consequences of these adaptations.
Whether it’s through the potential enhancement of cognitive performance or the mitigation of mood swings, the ramifications of this study stretch far beyond academic curiosity. It demands a reassessment of the biological challenges faced by menstruators and pushes the medical community to prioritize research that acknowledges and responds to these profound shifts. Ultimately, the narrative of menstruation—as a purely reproductive function—must evolve, articulated instead as a vital component of neurological health. This awakening in research opens pathways to understanding mental health within an enriched, holistic context, ripe for exploration and discourse in the scientific community.

Leave a Reply