Aging is a complex phenomenon that interacts intricately with our health, notably in the realm of cancer risk. Recent research has illuminated the dual nature of cancer susceptibility as we age, presenting a paradox that requires deeper understanding. While the risk of cancer escalates significantly during the 60s and 70s due to the accumulation of genetic mutations, astonishingly, evidence suggests that this risk may decline after reaching the age of approximately 80. This article aims to explore new findings that shed light on this counterintuitive trend and their implications for cancer research and treatment.
The human body undergoes myriad changes over its lifetime. The confluence of genetic mutations, environmental influences, and lifestyle choices contributes to the increased prevalence of cancer in older adults. This well-documented phenomenon can be attributed to the gradual and, often relentless, production of mutagenic factors. However, research conducted on mice has introduced significant insights into the declines in cancer risk observed in the oldest segments of the population.
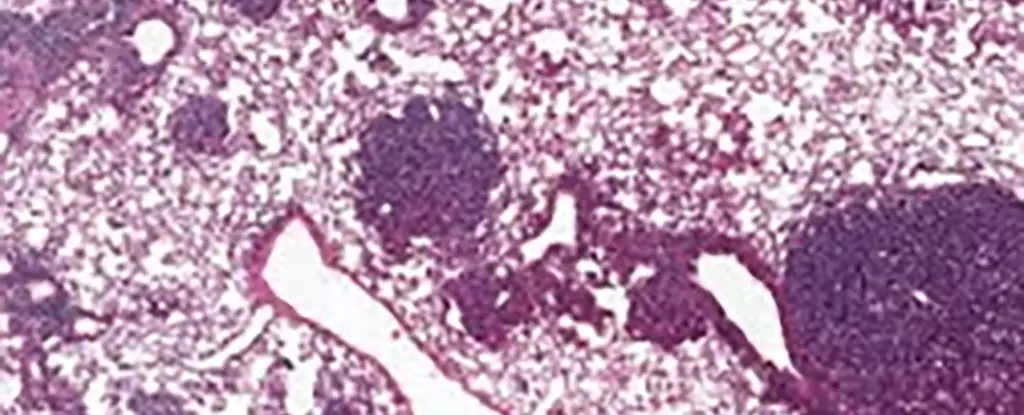
The findings from an international team of scientists, particularly focusing on lung cancer, illustrate the behavior of specific stem cells known as alveolar type 2 (AT2) cells. These cells are critical for the lung’s regenerative capacity and, as such, are pivotal in understanding tumor genesis. As AT2 cells age in mice, higher concentrations of a protein known as NUPR1 were noted, a pivotal factor in cellular behavior.
One of the most striking elements of the study is the relationship between NUPR1 and iron metabolism in aging cells. Researchers found that while aging cells possessed elevated iron levels, their functionality paradoxically mirrored a state of iron deficiency. This conundrum arose due to the increased presence of NUPR1, which inhibited the cells’ regenerative capabilities, ultimately limiting both healthy cellular growth and tumor proliferation.
According to Xueqian Zhuang, a prominent cancer biologist involved in this research, “Aging cells lose their capacity for renewal and therefore for the runaway growth that happens in cancer.” This phenomenon raises critical questions regarding the biological mechanisms that underpin aging and its subsequent effects on health, signaling a possible turning point for therapeutic interventions.
The implications of NUPR1’s effects are vast. As researchers delve deeper into the relationship between iron metabolism and cellular function, a potential vein of treatment avenues emerges. For instance, manipulating levels of NUPR1 or iron in cells could renew growth capabilities, opening pathways for treatments specifically targeting older populations. This approach is particularly timely given the rising number of individuals suffering from long-term consequences of diseases such as COVID-19, where lung function restoration is critical.
Another notable perspective derived from this study is the role of ferroptosis, a particular form of cell death linked to iron levels. Aging cells exhibit a functional deficiency in this process, potentially rendering them resistant to therapies designed to exploit ferroptosis. As Tuomas Tammela, another researcher from the study, emphasized, the timing of therapeutic intervention becomes critical: “The earlier ferroptosis treatment can be deployed, the more effective it’s likely to be.”
The cumulative research emphasizes a pivotal aspect of cancer prevention; the higher risk events occurring earlier in life might be significantly more consequential than previously acknowledged. It accentuates the importance of preventive measures, especially in youth, highlighting the necessity for programs that curtail smoking and exposure to other carcinogenic factors.
Furthermore, with the burgeoning field of personalized medicine, it’s essential to consider individual factors such as age, health conditions, and cancer type when devising treatment strategies. The research underscores that a nuanced understanding of aging’s impact on cancer biology is essential for developing targeted and effective interventions.
The intricate relationship between aging and cancer risk is beginning to unfurl, revealing a spectrum of possibilities for treatment and prevention. As researchers continue investigating the cellular and molecular underpinnings at play, the findings related to NUPR1, iron metabolism, and stem cell behavior present new avenues for combating cancer across various life stages. The journey of understanding these complexities positions us at the frontier of innovative cancer management, emphasizing once more the significance of personalized approaches in healthcare.

Leave a Reply