In the relentless battle against infectious diseases, understanding the mechanics of how pathogens spread is paramount. The COVID-19 pandemic illuminated this truth vividly, revealing that microscopic viruses can rapidly transform societies and economies. This collective wake-up call underscores a fundamental lesson: controlling an outbreak isn’t solely about medical treatment but hinges on dissecting how infections propagate through populations. The concept of R0, or the basic reproduction number, emerges as a crucial discriminator—highlighting the potential virulence and contagiousness of pathogens. When R0 exceeds one, the infection tends to expand exponentially, turning manageable outbreaks into devastating epidemics. Conversely, if R0 falls below one, natural decline often ensues, allowing disease control efforts to succeed. This mathematical insight is more than academic; it’s a blueprint for public health policies, vaccination strategies, and community interventions that can tip the scales toward safety.
Fomites and Invisible Pathways of Transmission
A vivid example of how seemingly innocuous objects can be silent carriers comes from the film *Contagion*, where a character stresses the importance of fomites—everyday inanimate objects like doorknobs, water fountains, and elevator buttons. These objects serve as covert conduits, harboring infectious agents long enough for another individual to touch and become infected. The importance of this insight became even clearer during pandemic-related sanitation campaigns. Recognizing the role of surfaces has transformed hygiene practices worldwide; frequent handwashing, disinfection, and barrier methods are now widespread strategies to limit disease spread. Moreover, the transmission route shapes the very nature of containment: airborne pathogens like measles demand rigorous airborne precautions, while contact diseases like Ebola require meticulous attention to bodily fluids. Understanding these transmission pathways empowers individuals and communities to implement targeted measures, transforming knowledge into practical actions that save lives.
The Contagious Spectrum: From Measles to Meningitis
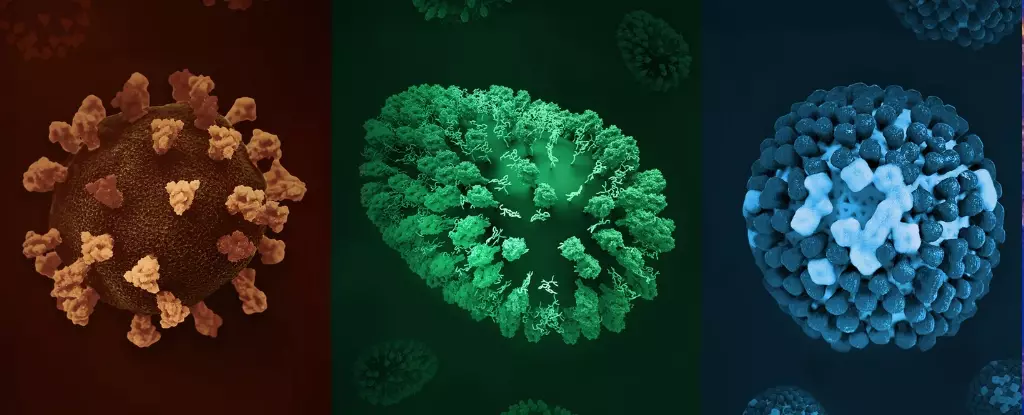
Some pathogens defy imagination with their infectiousness. Measles epitomizes this, with an R0 between 12 and 18—a striking figure that underscores its extreme contagion level. It can spread through microscopic airborne particles, remaining viable in the air for hours, and infecting even unvaccinated individuals who merely enter a room where an infected person was present hours earlier. This virulence explains the dramatic outbreaks seen worldwide, especially when vaccination rates dip due to misinformation or socio-economic disruptions. The power of vaccination in this context cannot be overstated; it acts as a biological firewall, dramatically reducing R0’s effective value. Similarly, pertussis (whooping cough), chickenpox, and COVID-19 exhibit high R0 values, making their control a constant challenge. These diseases aren’t just deadly—they are masters of rapid proliferation. Yet, their pathogenic prowess is countered through vaccines, public health measures, and societal awareness, demonstrating that understanding their spread provides us with tools to confront them.
The Quiet Threat of Slow Spread and Chronic Infections
While high R0 pathogens garner media attention, diseases with lower infectivity rates wield an insidious influence through persistence and complexity of treatment. Tuberculosis exemplifies this—its R0 varies roughly from less than one to four, heavily influenced by social determinants like overcrowding and healthcare access. Its transmission requires prolonged close contact, often within households or marginalized communities. The sobering reality of TB lies in its tenacity; it can lie dormant and then reawaken, necessitating long-term antibiotic regimens that challenge compliance and promote drug resistance. These traits make TB a formidable foe; even a relatively low R0 doesn’t diminish its potential to cause widespread suffering and death. This underscores a vital lesson: the infectivity of a pathogen isn’t the sole consideration—its capacity for persistence, resistance, and integration into social fabrics determines its overall threat.
The Risks and Realities of Less Contagious Diseases
On the other end of the spectrum lie diseases like Ebola, MERS, bird flu, and leprosy, with R0 values below one. Despite their lower transmissibility, these pathogens can be devastating. Ebola’s high fatality rate and the need for close contact for transmission paint a picture of a pathogen that, although less infectious, merits vigilance. Leprosy, with its slow progression and low R0, often lurks unnoticed for years, yet its social stigma and chronic disability make it a persistent threat in vulnerable regions. The key takeaway is clear: low R0 does not equate to low danger. The severity of outcomes, the difficulty of treatment, and the societal consequences amplify these diseases’ risks. Public health strategies must therefore remain vigilant across the entire spectrum, recognizing that the potential for devastation isn’t solely about how quickly a disease spreads, but also about how deeply it affects individuals and societies.
Strategies for a Safer Future
Ultimately, the control of infectious diseases hinges on our collective understanding and proactive measures. Vaccination remains the most potent weapon—building herd immunity to shield those who are most vulnerable, including infants, pregnant women, and immunocompromised individuals. However, vaccines alone aren’t enough; public education, hygiene practices, contact tracing, and response readiness form an interconnected web that can contain outbreaks before they spiral beyond control. Moreover, we must confront misinformation and vaccine hesitancy head-on, recognizing that the battle extends beyond biological science into the realms of policy, communication, and social cohesion. As the COVID-19 pandemic has painfully revealed, our resilience depends on not just reactive measures, but on foresight—the capacity to anticipate, understand, and outmaneuver the spread of unseen microbial foes. Only by harnessing the power of scientific insights and community efforts can we hope to mitigate the immense threat posed by infectious diseases moving forward.

Leave a Reply