Recent experiments have unveiled an astonishing breakthrough in neuroscience, specifically regarding the restoration of brain activity after cardiac arrest. A team of researchers from China has demonstrated the capability to reactivate neural functions in pigs nearly an hour after blood circulation halted. The study not only reveals that some brain functionalities can endure for hours post-arrest but also raises pivotal questions about the mechanisms of reviving brain function after significant medical emergencies, particularly sudden cardiac arrests.
Traditionally, cardiac arrest results in immediate cessation of blood flow, leading to ischemia— a condition characterized by insufficient oxygen and nutrient supply to an organ. Particularly concerning is cerebral ischemia, which can inflict irreversible damage to brain tissue within minutes. The critical window for resuscitation has long been alarmingly short, typically ranging from a few minutes to around ten, as prolonged ischemia becomes a formidable enemy to brain integrity. However, the recent discovery could potentially alter existing paradigms related to emergency medical protocols.
One of the striking revelations from this study is the integral role of the liver in maintaining and potentially restoring brain function post-cardiac arrest. The researchers proposed an innovative strategy that blends the functionalities of an undamaged liver with standard life support systems during resuscitation efforts. The liver, known for its detoxification capabilities, appears to hold significant potential in bolstering the recovery of the brain after ischemic events.
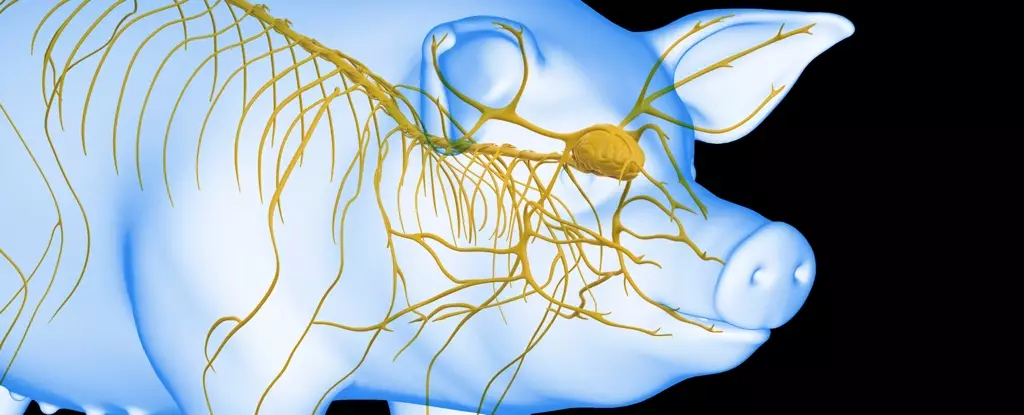
In their experiments, researchers utilized Tibetan minipigs to simulate various conditions of ischemia. By segregating the subjects into distinct groups—some experiencing liver ischemia, while others did not—the team was able to draw compelling conclusions about the protective role of the liver during brain revival. Notably, pigs that underwent brain ischemia without liver ischemia exhibited less damage compared to those subjected to both ischemic conditions. This underscores the liver’s potential in mitigating neurological damage following cardiac arrest.
Innovative Experimental Methodology
To explore this hypothesis deeper, the researchers embarked on ambitious experiments involving the integration of an undisturbed pig liver into a life support apparatus meant for brain revival. While this approach may not apply directly to human practices, the insights derived from this experimental design are invaluable. The team employed an artificial heart and lungs to circulate fluids while observing the subsequent neural activity.
Conducting the trials, they connected the brain to the life support system at varying intervals post-ischemia. Each assessment gleaned fascinating results, particularly with the liver-assisted technique, which substantially extended the viability of brain activity post-ischemia. When brains were connected to the liver-integrated system within 50 minutes post cessation, electrical activity resumed, lasting impressively for six hours. This stark contrast with the outcomes of the system without liver assistance illustrates the critical role the liver may play in post-arrest resuscitation.
These findings have profound implications for the future of emergency medicine and the management of cardiac arrest incidents. The evidence suggests that integrating liver functionality into resuscitation tools can significantly prolong the time doctors have to revive brain function after an arrest. As researchers continue to explore this trajectory, there lies hope for improving survival and recovery rates among patients who face similar life-threatening scenarios.
Furthermore, the understanding garnered from such studies can inspire fresh research initiatives aimed at uncovering novel therapeutic techniques that could minimize brain injuries during cardiac arrest events. The prospect of extending the resuscitation window opens the doors to designing more sophisticated medical interventions that could ultimately save lives.
This revolutionary research highlights the need for a paradigm shift in our understanding of cardiac arrest recovery and brain health preservation. Acknowledging the liver’s role could redefine emergency response protocols, fostering better outcomes for patients post-cardiac arrest. With further studies extrapolating these promising results, we stand at the cusp of potentially transformative advancements in resuscitation practices that could improve the odds of survival in critical care settings. The integration of multi-organ support in resuscitation strategies may soon become a cornerstone of modern medicine, paving the way for a new era in neuro-recovery.
Leave a Reply