Recent research has unveiled a promising frontier in cancer treatment, specifically through the optimization of immunotherapy by employing the body’s dual immune responses. This approach challenges traditional understandings of immune functionality in the context of cancer, suggesting that the relationship between various immune responses might be more intricate than previously thought. Rather than merely relying on the conventional methods of enhancing Type 1 immune responses to combat cancer cells, scientists are beginning to explore the synergistic potential of combining both Type 1 and Type 2 responses, leading to groundbreaking insights that could reshape therapeutic protocols.
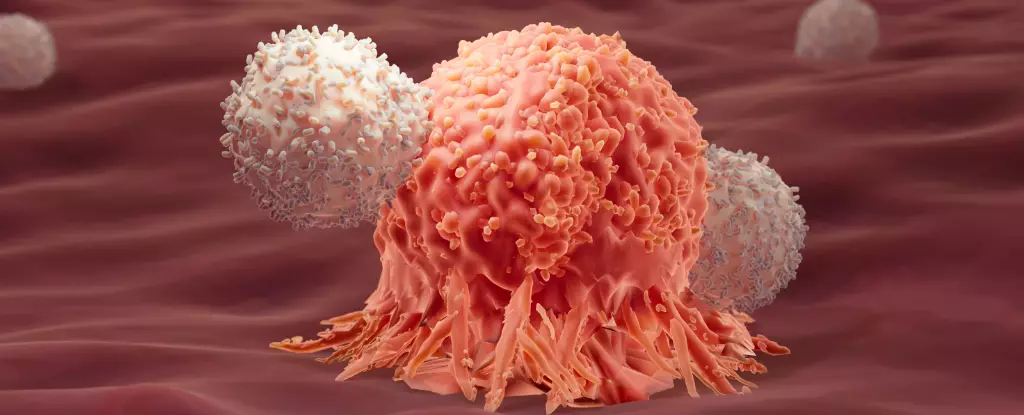
The immune system has long been recognized as a powerful adversary against malignancies, leveraging various mechanisms to detect and destroy aberrant cells. Immunotherapy, particularly chimeric antigen receptor T-cell (CAR-T) therapy, has emerged as a beacon of hope for the treatment of certain blood cancers like leukemia. However, its efficacy has met with limitations, particularly in the case of patients experiencing relapse after initial successful treatment. Researchers from the École Polytechnique Fédérale de Lausanne (EPFL) have embarked on a quest to elucidate why some patients achieve remarkable long-term remissions while others face relapse.
Significantly, their investigations centered on the immune signatures of patients who have been in remission for extended periods—extending up to eight years. By analyzing a robust genetic database from 82 patients involved in two early clinical trials, the team discovered a surprising prevalence of markers associated with Type 2 immune responses. Conventional wisdom had relegated this immune avenue to be inconsequential or even detrimental in the cancer context, primarily thought to combat larger threats like parasites. However, a curious correlation emerged, suggesting that these Type 2 markers might play a role in sustaining cancer remission.
To validate their findings, researchers ventured into experimental animal models. Using mice with pre-existing tumors, they conducted trials comparing conventional Type 1 immunotherapy to a composite treatment that combined both Type 1 and Type 2 responses. The results were revealing: a staggering 86% of the mice receiving the dual treatment achieved remission, while those subjected solely to Type 1 therapies did not survive beyond a few weeks following treatment.
This success prompted an exploratory investigation into how Type 2 immune components could enhance the effectiveness of anticancer immunity, particularly in solid tumors that notoriously resist immunotherapy. Analysis indicated that modified Type 2 proteins facilitated a biochemical pathway known as glycolysis. The activation of this pathway appears to provide T cells with a much-needed energy surge, enabling them to endure the metabolic stress typically imposed by battling solid tumors.
The interplay of Type 1 and Type 2 immune responses can be visualized through the lens of the yin and yang philosophy—each response, although distinct, possesses unique strengths and when harmonized, can yield superior outcomes in the relentless fight against cancer. The findings from the EPFL studies articulate a compelling narrative for rethinking therapeutic strategies, urging a departure from the binary distinction between immune types.
Li Tang, a co-author on the studies, articulated the necessity of this new perspective: “Our results show that Type 1 and Type 2 immunity can be thought of in terms of synergy.” This viewpoint not only opens avenues for novel immunotherapies but also advocates for a more holistic understanding of the immune defense system, encapsulating its vast and dynamic capabilities.
The revelations stemming from these studies are poised to revolutionize the landscape of cancer immunotherapy. As researchers delve deeper into the mechanisms behind this dual immune response synergy, there lies vast potential for developing refined treatment regimens that could improve patient outcomes significantly. Such therapies could be designed to exploit the metabolic advantages conferred by Type 2 responses while concurrently deploying aggressive Type 1 tactics against cancer cells.
These findings represent a clarion call within the scientific community to reexamine and embrace the complexity of immune interactions. By fostering an integrative approach that leverages the strengths of both immune pathways, we may be on the cusp of unlocking new possibilities in cancer treatment, offering hope to countless patients who grapple with this formidable disease. The next few years will be crucial as this research transitions from lab bench to clinic, promising a future where dual immune response strategies enhance survival rates and prolong remissions in cancer care.

Leave a Reply