In a groundbreaking development that could redefine the approach to neurodegenerative diseases, a novel drug has emerged, targeting inflammation in the brain while simultaneously strengthening the blood-brain barrier in mice. The research, spearheaded by pathologist Sanford Markowitz from Case Western Reserve University, has unveiled an exciting realm of possibilities that may transform the therapeutic landscape for conditions such as Alzheimer’s disease. As traditional methods have often revolved around the removal of amyloid proteins, this alternative seeks to address underlying inflammation, a critical factor in maintaining cognitive health.
Rethinking Alzheimer’s Treatment
Alzheimer’s treatment has long revolved around a singular focus: the abnormally clumping amyloid proteins. However, the recent discovery that the new drug, which inhibits an immune protein known as 15-PGDH, does not alter amyloid levels yet still enhances the integrity of the blood-brain barrier is revolutionary. Markowitz argues that inhibiting this particular enzyme presents a fresh perspective on treating Alzheimer’s, distinct from existing drugs that frequently result in undesirable side effects and limited efficacy. The traditional narrative of “remove the amyloid” is outdated, and this novel approach could herald a decisive shift toward more holistic solutions that prioritize brain health.
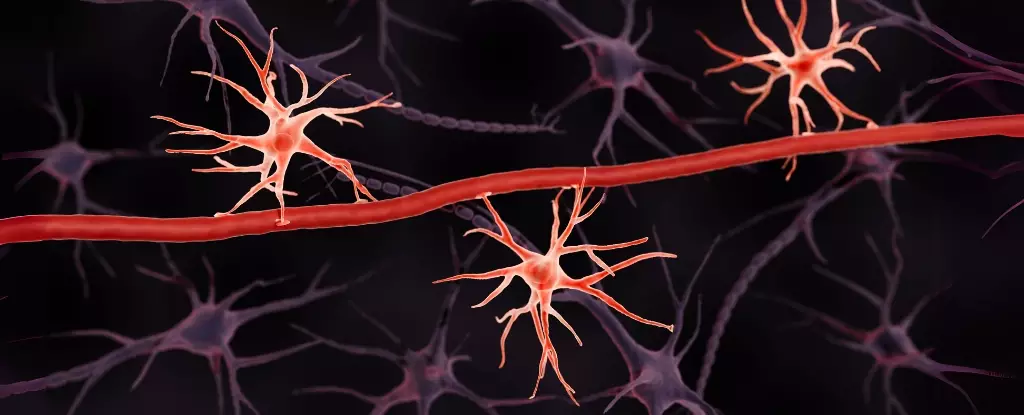
The Role of the Blood-Brain Barrier
The blood-brain barrier serves as a crucial protective shield, filtering harmful entities such as toxins and pathogens from entering the brain. Its deterioration is often the harbinger of cognitive decline and is especially prevalent in conditions such as Alzheimer’s. The pivotal study conducted by Markowitz and his colleagues, including physiologist Yeojung Koh, adds dimension to prevailing concepts surrounding the blood-brain barrier’s role in neurodegeneration. Their work illustrates how traumatic brain injuries compromise this protective layer, leading to heightened susceptibility to cognitive disorders. By understanding the molecular dynamics within the barrier, researchers could not only prevent damage but also promote recovery in affected individuals.
SW033291: A New Frontier
The compound SW033291, developed to inhibit the activity of 15-PGDH, represents a novel pharmacological intervention targeting the preservation of cognitive functions post-injury. In experimental models, mice treated with this drug exhibited unwavering memory and cognition, even in the wake of significant traumatic brain injuries. Neuroscientist Andrew Pieper emphasizes the importance of these outcomes, branding the results as “remarkable.” The blood-brain barrier remained intact, serving as a testament to the compound’s effectiveness and opening the door to further exploration of similar treatments.
A Call for Innovative Research
Despite the staggering statistic of nearly 10 million new dementia cases annually, traditional research methodologies in this domain have often yielded unsatisfactory results. The shift toward exploring inflammation and immune response as therapeutic targets signifies a refreshing change in focus. Markowitz and his team’s assertion that 15-PGDH serves as a guardian of the blood-brain barrier aligns with a growing narrative that encourages researchers to think outside conventional parameters. As the implications of these findings unfold, the potential for broader applications in neurodegenerative treatment presents an exciting frontier that warrants continued exploration. The journey may still be long, but the promise of safeguarding cognitive health through innovative approaches has never been more palpable.

Leave a Reply