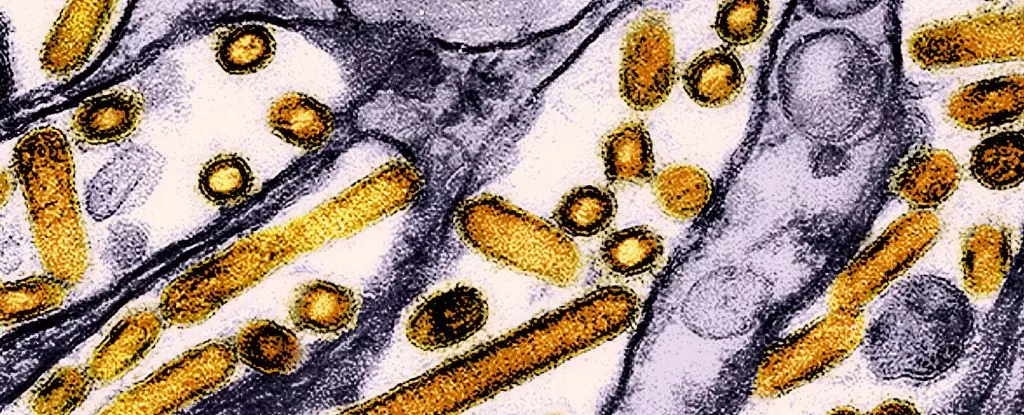
Recent studies conducted by researchers from the US Centers for Disease Control and Prevention (CDC) have unveiled shocking revelations about the presence of highly pathogenic avian influenza (HPAI), specifically the H5N1 strain, among dairy workers in the United States. Blood samples collected from 115 dairy workers across Michigan and Colorado between June and August 2024 revealed alarming results: 7 percent of those tested carried antibodies indicative of previous exposure to the virulent bird flu. This information, while initially concerning, also ensures that the majority of those infected have not experienced severe symptoms, with approximately half of antibody-positive individuals reporting no illness at all.
The implications of such discoveries are multifaceted. While it appears that most dairy workers have been able to fend off severe illness from the virus, the underlying cause for alarm lies in the potential for the virus to mutate and lead to more dangerous strains. This pattern of mild infection combined with the virus’s capacity for mutation poses significant public health challenges. The current situation emphasizes the need for robust monitoring and immediate interventions to mitigate risks.
In Cambodia, a concerning outbreak has already demonstrated the potential dangers of avian influenza mutations. Reports indicate that three individuals have died after contracting a hybrid strain of the H5N1 virus, believed to have mutated to enhance airborne transmission—a stark reminder that the disease’s virulence can suddenly intensify. This emerging hybrid strain combines known variants and showcases mutations that enhance its ability to infect mammals, raising red flags for global health authorities.
The Canadian instance of bird flu, in which a teenager has fallen critically ill with a mutated version originating from a dairy cow outbreak in the US, offers further cause for concern. Preliminary genetic investigations indicate changes in a gene closely associated with the virus’s capacity to infect humans, highlighting the mutable nature of H5N1 and its potential to threaten human health. While officials believe this case remains isolated, it notably underscores the necessity for guarded vigilance and strategic management of avian flu outbreaks.
The findings regarding the dairy workers illuminate pertinent aspects of occupational health and safety. All identified cases of human infection linked to the H5N1 strain involved individuals who were directly engaged in milking cows or cleaning dairy facilities. Notably, none of these workers utilized personal protective equipment (PPE) recommended for handling HPAI-infected animals. This alarming discovery underscores systemic issues regarding workplace safety measures and the need for enhanced training and personalized outreach programs tailored to culturally specific workforce demographics, particularly as many affected workers are Spanish-speaking.
Moreover, the symptoms associated with the infections—ranging from typical flu-like indicators such as fever and sore throat to more peculiar symptoms including itchy eyes and headaches—demonstrate the necessity for health agencies to rapidly develop awareness initiatives. Improvement in the use of PPE among these workers is paramount, and healthcare providers must ensure thorough education regarding the symptoms of HPAI exposure.
In the United States, the current climate surrounding HPAI has led to the infection of over 400 dairy herds across 48 states since the outbreak began in 2022, resulting in the culling of approximately 90 million domestic birds. Such drastic measures highlight the critical importance of monitoring and managing the impact of this virus on poultry and other animal populations.
Experts are advocating for continuous and intensified surveillance of both avian and human health to avert further outbreaks. This includes not only monitoring bird populations but also watching for signs of infection among at-risk communities. Health authorities worldwide are emphasizing the necessity for robust hygiene practices when interacting with animals and instituting reporting mechanisms for cases of multiple sick or dead birds.
As part of a comprehensive response strategy, wildlife protection programs are also being put into place. For instance, California’s efforts to vaccinate condors against avian flu serve as a crucial step in safeguarding endangered species while concurrently combating the virus’s spread. Furthermore, ongoing research into developing a human vaccine against H5N1 is imperative—an effort that could protect both workers and the broader community from potential pandemics.
The emergence of almost undetected cases of avian influenza in human populations, particularly among dairy workers, highlights the imperative need for increased public health vigilance and proactive measures. As we closely monitor the dynamic landscape of avian influenza and the various outbreaks worldwide, the lessons learned from these recent findings must be used to foster better protection for both workers and vulnerable animal populations. Stakeholders must rally together—healthcare authorities, agricultural employers, and communities—to ensure thorough education, adequate resources, and effective response strategies to navigate the complexities of this evolving public health challenge.

Leave a Reply