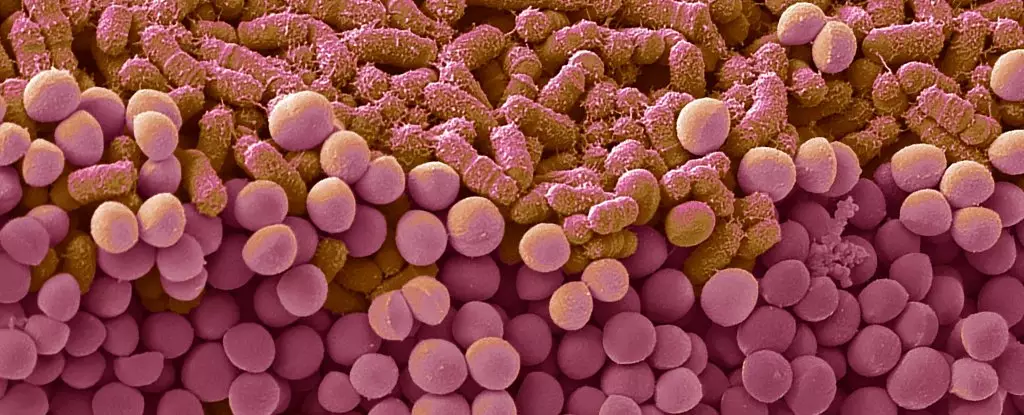
For decades, dieting has been shrouded in frustration and disappointment, primarily because so many struggle to maintain their weight loss. The notorious “yo-yo effect,” where individuals oscillate between losing weight and gaining it back, has long been considered a purely behavioral or metabolic challenge. Yet, emerging research suggests that the root of this cyclical struggle might be seated much deeper—embedded within the microscopic ecosystem residing in our digestive tracts. Specifically, our gut microbiota, the diverse community of bacteria inhabiting our intestines, appears to play an instrumental role in dictating our eating habits and, consequently, our ability to sustain healthy weight loss.
In dissecting this complex relationship, recent experiments conducted by researchers in France have shed illuminating light on how dieting patterns impact gut bacteria, which in turn influences our craving for unhealthy foods and perpetuates weight cycling. Their findings go beyond conventional wisdom, revealing that the gut’s microbial composition doesn’t merely adapt in response to diet but may also encode behaviors that make future dieting efforts more arduous. This interconnectedness hints at an entirely new perspective: successful weight management might hinge less on willpower alone and more on understanding the biological symphony playing out beneath our awareness.
The Microbiome’s Role in Reinforcing Unhealthy Eating Habits
The researchers designed a series of experiments with mice to simulate the effects of yo-yo dieting, alternating the animals’ diets between nourishing standard meals and high-fat, sugar-laden fare emblematic of Western dietary patterns. What they observed was startling. After periods of overeating, which mimicked indulgent dieting phases, returning to healthier diets triggered binge-like behaviors in these mice. Not merely temporary cravings, but sustained episodes driven by a shift in the bacterial population within the gut. This change was not superficial; it altered their metabolism in ways that predisposed them toward overeating—creating a vicious cycle that could, in theory, persist indefinitely.
Even more compelling was the discovery that transferring these altered bacteria to other mice—who had no prior dieting history—induced the same binge behaviors. This pivotal experiment demonstrated that shifts in microbiota could directly influence eating patterns, independent of a person’s conscious choices. Essentially, a change in gut bacteria could be rewiring the brain’s reward pathways, making food pleasurable beyond actual hunger, thus tethering eating to emotional and hedonic triggers rather than nutritional needs.
What this implies is profound: dieting, particularly if inconsistent or cyclical, may inadvertently entrench the very behaviors it seeks to eradicate. The microbiota, once altered, could be hijacking the brain’s desire for rewarding foods, making sustained dietary change increasingly difficult. This line of inquiry challenges the traditional focus solely on calorie counting and behavioral modification, urging us to consider the biological underpinnings that shape our relationship with food.
Implications for Future Weight Management Strategies
The insights from this research serve as a wake-up call to the conventional approach to weight loss. If our gut bacteria are actively reinforcing binge behaviors, then addressing weight struggles requires a paradigm shift—from solely focusing on willpower and calorie restriction to also targeting the microbiome. This could involve developing therapies designed to modify the gut’s bacterial composition, restoring a microbial balance that supports healthier eating behaviors and metabolism.
Moreover, these findings open doors to personalized medicine. Since each individual’s microbiome is unique, interventions could be tailored to modify specific bacterial strains implicated in binge eating, offering a more precise and potentially more effective approach. This would be a departure from one-size-fits-all dieting advice, moving toward microbiome-centered treatments that could help break the cycle of yo-yo dieting once and for all.
Yet, caution remains necessary. Much of the current evidence is drawn from animal models, and translating these findings into human applications must be approached with rigorous clinical trials. Still, the potential is undeniable; understanding and manipulating the microbiome could emerge as a cornerstone in combating obesity, not merely by reducing calorie intake but by addressing the biological drivers of unhealthy eating patterns.
The genetic and environmental factors shaping our gut microbiota are vast, but this research makes it clear that our microbial inhabitants are not passive passengers—they are active players in our health journey. Recognizing their influence marks a shift toward a more holistic, biologically informed approach to weight management. With continued investigation, the hope is that future therapies will not only help individuals shed pounds but also establish sustainable, healthy eating habits that resist the allure of the microbiome’s addictive reach.

Leave a Reply